Recent Posts
How Doctors Monitor and Manage Perimenopause Symptoms

Perimenopause is a natural stage in a woman’s life, but that doesn’t mean it’s easy. It’s the transitional period leading up to menopause, marked by fluctuating hormones, irregular cycles and a wide range of physical and emotional changes. While the experience varies from woman to woman, for many, it can bring symptoms that affect their daily lives and well-being.
If you're in your 40s and starting to notice changes in your body or mood, you may be entering perimenopause. The good news is that your doctor can help you navigate this phase with the support, tools and treatments you need to feel like yourself again.
What Is Perimenopause?
Perimenopause refers to the time before menopause when a woman’s hormone levels begin to shift. Estrogen and progesterone, the two primary female hormones, start to fluctuate, causing menstrual cycles to become irregular. This phase can last anywhere from a few months to several years and typically begins in a woman’s 40s, though it can start earlier.
Menopause is officially diagnosed when a woman has gone 12 consecutive months without a menstrual period. Perimenopause ends at that point, but the symptoms and changes often begin well before that milestone.
Common Symptoms of Perimenopause
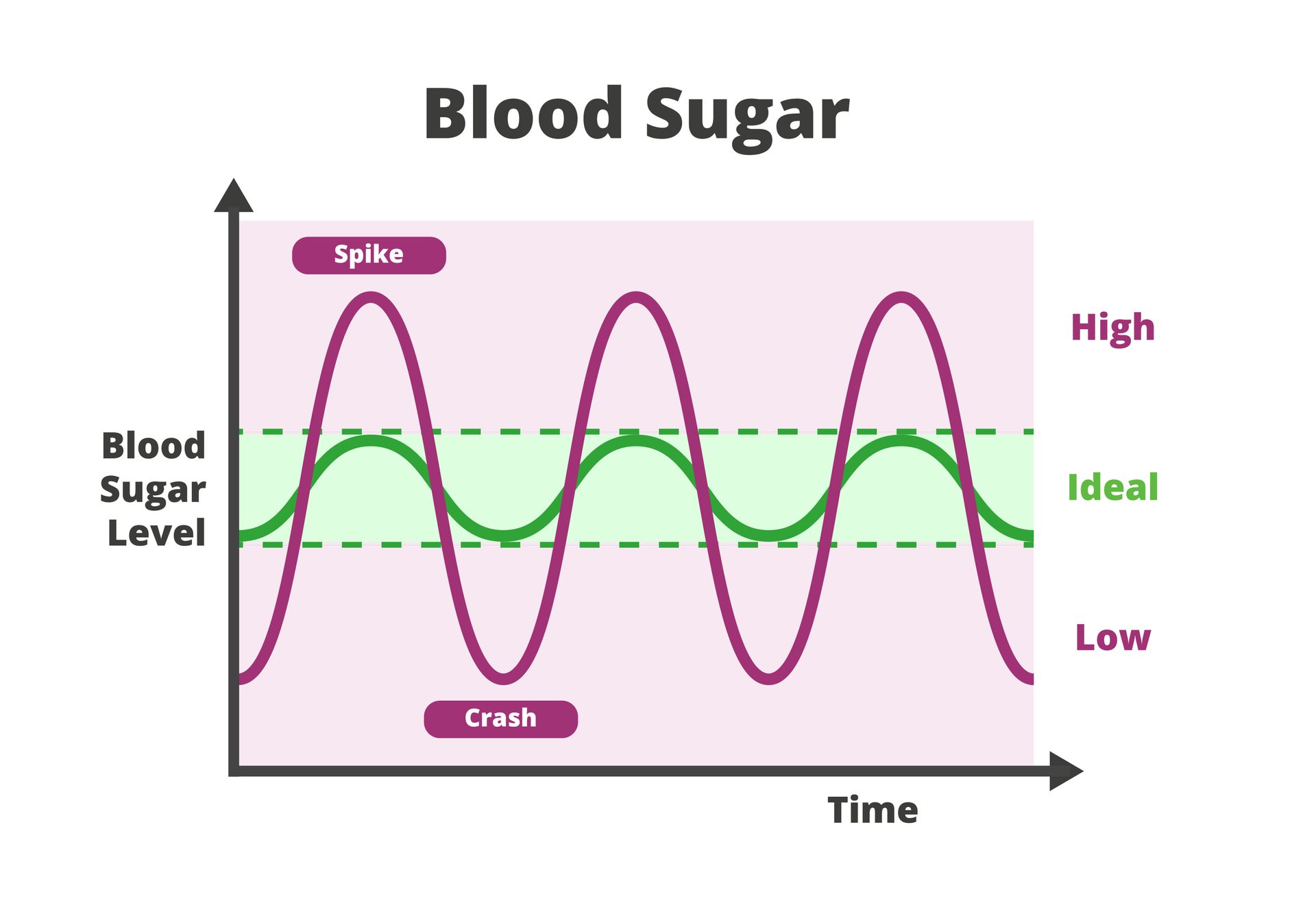
Because hormone levels rise and fall unpredictably during perimenopause, symptoms can be wide-ranging and inconsistent.
Some of the most common include:
- Hot flashes or night sweats
- Irregular periods
- Mood swings, anxiety or depression
- Sleep disturbances
- Vaginal dryness or discomfort during sex
- Brain fog or memory issues
- Fatigue
- Weight gain, especially around the abdomen
- Decreased libido
These symptoms may be mild for some women and more disruptive for others. Regardless of severity, it’s important to talk to your doctor if you’re experiencing changes that affect your quality of life.
How Doctors Monitor Perimenopause
Symptom Assessment
Your doctor will start by asking about your menstrual history and current symptoms. Keeping a journal of your cycles, mood changes, sleep patterns and other symptoms can be very helpful during your visit. This helps your doctor understand the patterns and determine how your symptoms may be linked to hormonal changes.
Blood Tests
While there’s no single test that can definitively diagnose perimenopause, your doctor may order blood work to check levels of:
- Follicle-Stimulating Hormone (FSH):
High levels may indicate your ovaries are slowing down.
- Estrogen:
Fluctuating estrogen levels are a hallmark of perimenopause.
- Thyroid Function: Since thyroid issues can mimic perimenopausal symptoms, doctors often do tests to ensure a thyroid issue isn’t misdiagnosed as perimenopause.
- Other Hormones: Depending on your symptoms, your doctor may test progesterone or testosterone levels.
It’s important to note that hormone levels can vary from day to day, so a diagnosis is often made based on a combination of test results and clinical symptoms.
How Doctors Manage Perimenopause Symptoms
The goal of treatment is to help you feel better and maintain your health through the transition. Treatment options are personalized based on your symptoms, age, medical history and lifestyle.
Lifestyle Recommendations
Doctors often start with lifestyle changes, some of which can provide significant relief without resorting to hormone therapy:
- Diet: Eating a balanced diet rich in calcium and vitamin D helps support bone health. Limiting caffeine, sugar and alcohol can reduce symptoms like hot flashes and mood swings.
- Exercise: Regular physical activity improves mood, sleep, weight management and energy levels.
- Sleep hygiene: Creating a calming bedtime routine and managing screen time can help address sleep disturbances.
Hormone Therapy
For women with moderate to severe symptoms, hormone replacement therapy (HRT) may be recommended. HRT replaces the estrogen your body is losing and can relieve hot flashes, night sweats and vaginal dryness. It also helps protect against bone loss.
Hormone therapy isn’t right for everyone, so your doctor will weigh the benefits and risks based on your personal and family health history.
Non-Hormonal Medications
If hormone therapy isn’t an option, your doctor may recommend other medications to address specific symptoms. These might include:
- Antidepressants: Low-dose antidepressants can ease mood swings and hot flashes.
- Sleep aids: Short-term use of sleep medications may be helpful for managing insomnia.
- Vaginal estrogen: Topical treatments can help with vaginal dryness without affecting the entire body.
Supplements and Alternative Therapies
Some women find relief with supplements like black cohosh or evening primrose oil, though their effectiveness varies. Your doctor can help you evaluate whether these are safe and appropriate for your situation.
Get Personalized Perimenopause Care in Houston
Perimenopause is a natural phase of life, but that doesn’t mean you can’t mitigate the symptoms or discomfort. With the right medical support, education and self-care strategies, you can manage your symptoms and maintain your quality of life.
At St. Hope Healthcare, we know how overwhelming perimenopause can feel. Our women’s health care providers take the time to listen to your concerns, answer your questions and create a care plan that supports your health and well-being during this important transition.
Schedule your women’s health visit today at St. Hope Healthcare by calling (713) 778-1300.