Recent Posts
The Role of Primary Care in Managing Menopause and Perimenopause
Menopause is a natural part of aging, yet for many women it brings physical, emotional and hormonal changes that can be difficult to manage alone. The years leading up to menopause, known as perimenopause, often come with unpredictable cycles, sleep issues, mood swings and other symptoms that may affect daily life. During this transition, your primary care provider plays an essential role in helping you navigate the changes safely and comfortably.
Primary care is not just for annual checkups. It serves as a long-term partnership focused on whole-person health. When it comes to menopause and perimenopause, your provider can help track symptoms, monitor your heart and bone health and support your mental well-being while making sure other underlying conditions are not overlooked.
Perimenopause and Menopause
Perimenopause typically begins in a woman’s 40s, though some may experience changes earlier.
Hormone levels fluctuate as the ovaries produce less estrogen and progesterone, leading to irregular periods, hot flashes, night sweats and mood changes. Menopause is officially reached when a woman has gone 12 consecutive months without a menstrual cycle.
While these changes are normal, their intensity and duration vary from person to person. That is why individualized care from a trusted provider is so important. Primary care professionals help patients recognize what is typical and when additional testing or treatment may be needed.
Tracking Symptoms and Health Changes
Your provider can help you track and interpret patterns in your symptoms over time. Keeping a journal of sleep quality, hot flashes, mood changes and cycle length can provide valuable information that supports diagnosis and treatment decisions.
Primary care visits during perimenopause are an opportunity to discuss how these symptoms affect your daily life and identify triggers that make them worse. For example, caffeine, alcohol and stress can increase the frequency or severity of hot flashes. Regular tracking allows your provider to recommend personalized strategies, such as dietary adjustments or medication options, to keep symptoms manageable.
Monitoring Blood Pressure and Heart Health
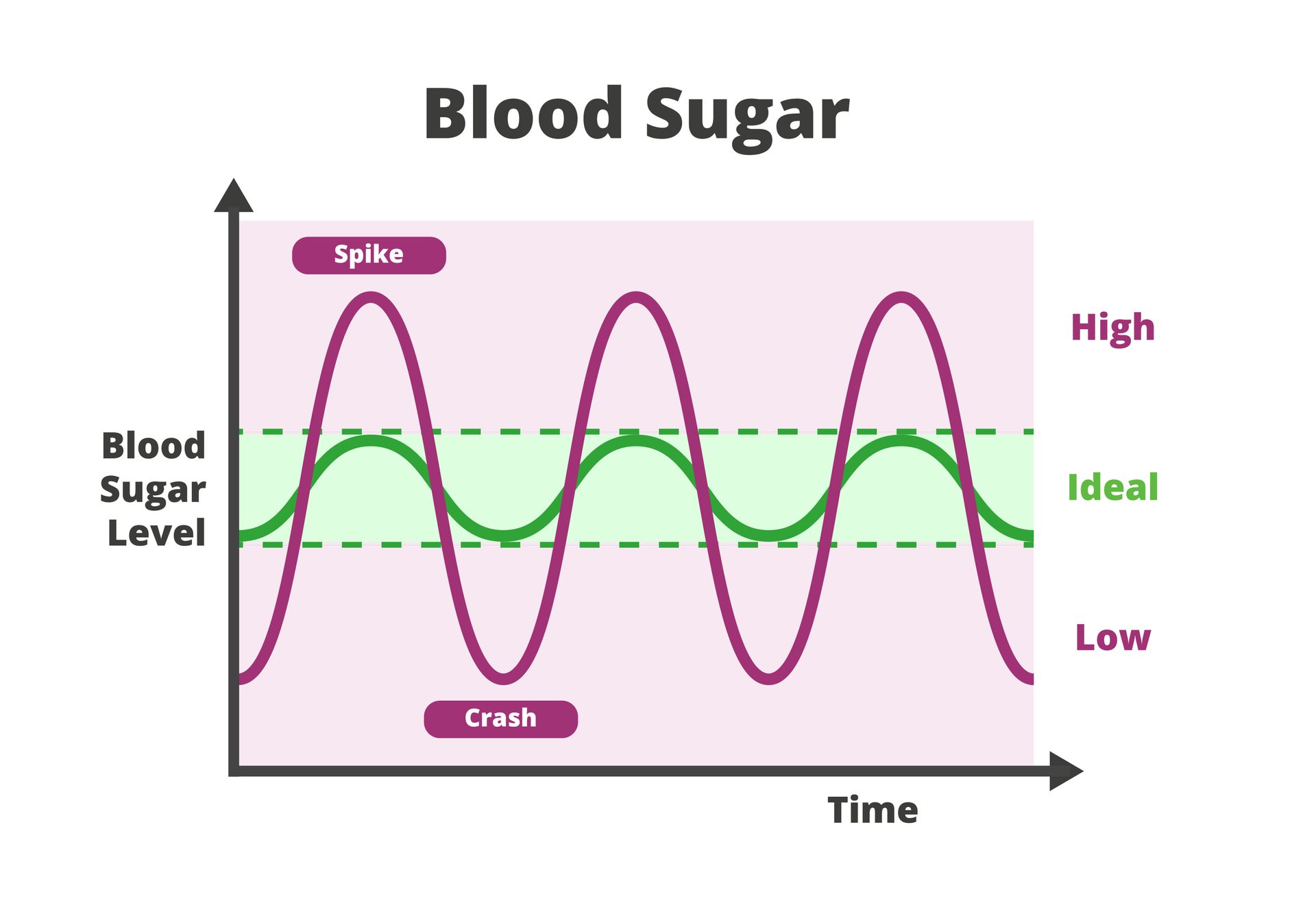
As estrogen levels decline, the risk of cardiovascular disease increases. Estrogen plays a protective role in keeping blood vessels flexible and supporting healthy cholesterol levels. During and after menopause, blood pressure and cholesterol can rise, making regular monitoring critical.
Your primary care provider will measure your blood pressure at each visit and may recommend blood tests to check cholesterol and glucose levels.
Supporting Bone Health
Bone loss accelerates after menopause due to lower estrogen levels, which can lead to osteoporosis and fractures if not addressed early. A primary care provider will assess your risk factors for bone thinning, such as family history, low calcium intake or a sedentary lifestyle.
Depending on your age and health history, your provider may recommend a bone density scan to evaluate your bone strength. They can also advise on proper calcium and vitamin D intake, strength-building exercises and lifestyle habits that help maintain healthy bones. In some cases, medications may be prescribed to slow bone loss or improve bone density.
Addressing Mental and Emotional Wellness
Menopause is not just a physical transition; it can affect mental health as well. Hormonal fluctuations may lead to mood swings, anxiety or depression. Some women also experience difficulty concentrating or changes in memory. These symptoms can be confusing and frustrating, especially when combined with sleep disturbances.
Your primary care provider is trained to recognize these emotional changes and help you find support. They may recommend counseling, stress management techniques or medication if depression or anxiety becomes severe.
Coordinating Care and Treatment Options
Primary care providers can coordinate care across different specialties when necessary. For instance, if your symptoms suggest a hormonal imbalance, your provider might collaborate with an endocrinologist or gynecologist. If you are struggling with bone health, they can refer you to a rheumatologist or recommend specific therapies.
This coordination helps prevent overmedication or conflicting treatment plans that sometimes happen when care is fragmented.
Receive Compassionate Menopause Care in Houston, TX
At St. Hope Healthcare, we know that every woman experiences menopause differently. Our caring primary care providers take the time to listen, track your symptoms and create a plan that supports your physical and emotional well-being.
Call St. Hope Healthcare at (713) 778-1300 to schedule your appointment.