Recent Posts
Is It Normal to Feel Burned Out Managing Your Diabetes?

From checking blood sugar levels and monitoring diet to remembering medications and scheduling checkups, managing diabetes can sometimes feel like a full-time job—because in many ways it is. That never-ending pressure can lead to a sense of frustration, exhaustion or even emotional detachment that many people describe as diabetes burnout.
Diabetes Burnout
Diabetes burnout happens when the daily demands of managing the condition start to feel overwhelming. You might find yourself skipping blood sugar checks, ignoring dietary guidelines or feeling resentful about the constant need for monitoring. These reactions are not signs of weakness or failure; they are human responses to chronic stress.
Managing diabetes takes persistence and discipline, often without breaks. There’s no vacation from checking blood sugar, planning meals or worrying about long-term complications. Over time, this level of responsibility can drain mental and emotional energy, especially if progress feels slow or setbacks occur.
Why Diabetes Burnout Happens
Constant Vigilance
Diabetes management is ongoing. Even when your numbers are stable, you have to think about what you eat, how you exercise and how your medications will interact with daily activities. That level of attention can wear anyone down over time.
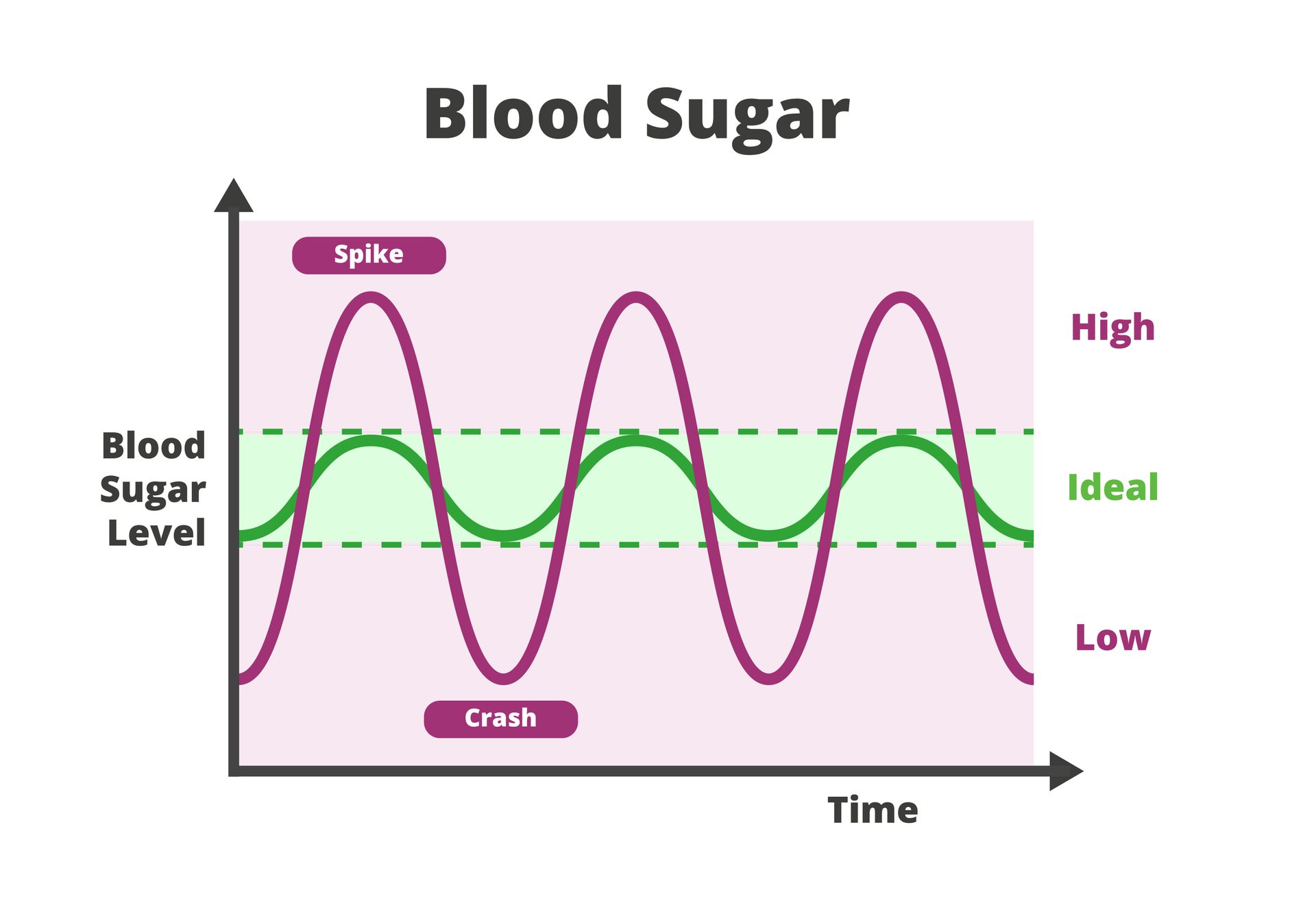
Unpredictable Results
You can follow your plan perfectly and still see unexpected blood sugar readings due to stress, illness or hormonal changes. Those fluctuations can make it feel like your hard work is not paying off.
Fear of Complications
Living with diabetes often means living with long-term worries about heart disease, vision loss or kidney issues. While these risks can be managed, constantly thinking about severe, life-altering consequences can increase anxiety and mental strain.
Lack of Support
When you feel like you’re managing diabetes alone, it can be harder to stay motivated. Without encouragement or understanding from family, friends or healthcare professionals, burnout can develop faster.
Emotional Fatigue
Diabetes affects more than your body; it affects how you feel, how you eat and how you interact with others. The emotional toll can accumulate over months or years, leading to mental exhaustion.
How Your Care Team Can Help
You do not have to face diabetes burnout by yourself. Your primary care provider and healthcare team are there to support both your physical and emotional health. They can help identify what’s causing your fatigue and create a realistic plan to make diabetes care more manageable.
Adjusting Your Care Plan
If you feel overwhelmed, your provider may simplify your routine or suggest new tools like continuous glucose monitors (CGMs) or mobile apps that reduce the burden of tracking. Small changes in medication schedules or meal planning can also make daily care easier.
Providing Emotional Support
Managing a chronic condition can take a toll on mental health. Your provider may recommend counseling, support groups or stress-reduction techniques to help you process the emotional side of diabetes. Sometimes, simply talking to someone who understands can make a big difference.
Encouraging Self-Compassion
Perfection is not the goal of diabetes care; consistency is. Your healthcare team can help you set achievable goals and remind you that occasional setbacks do not mean failure. Learning to forgive yourself for missed checks or slip-ups is part of maintaining long-term wellness.
Monitoring for Depression or Anxiety
Depression and anxiety are common among people managing chronic illnesses. If your provider suspects these are contributing to burnout, they can connect you with mental health specialists or provide treatment options.
Strengthening Your Support System
Your provider can also involve family members or caregivers in your care plan, helping them understand how to offer meaningful support without adding pressure. Feeling supported at home can make daily management feel less isolating.
Steps You Can Take at Home
- Celebrate small wins: Recognize progress, whether it’s improved readings, better sleep or consistent exercise.
- Stay connected: Join diabetes support groups or talk to others living with the condition. Shared experiences can make you feel less alone.
- Practice stress relief: Activities like walking, yoga, journaling or deep breathing can lower stress and improve focus.
- Prioritize sleep and hydration: Both play a major role in how your body regulates blood sugar and energy levels.
Get Help Developing a Sustainable, Less-Stressful Approach to Diabetes Management
If you are feeling burned out or overwhelmed by your diabetes management, the compassionate providers at St. Hope Healthcare are here to help. Schedule an appointment at one of our health centers in Bellaire, Conroe, Houston, Sugar Land and Dickinson online or call us at (713) 778-1300.