Recent Posts
What Houston Patients Should Know About GLP‑1 Medications for Diabetes and Weight Management

GLP‑1 receptor agonists, commonly known by brand names like Ozempic, Wegovy, Trulicity and Mounjaro, have become widely discussed for their dual benefits: helping control type 2 diabetes and, in many cases, enabling significant weight loss.
There’s one particularly big problem that makes obtaining GLP-1 medications difficult for many patients. They’re expensive, especially when prescribed outside of diabetes treatment. For Houston patients, particularly those using 501(c)(3) clinics and on Medicaid, navigating affordability and eligibility can be challenging.
How Do GLP‑1 Medications Work?
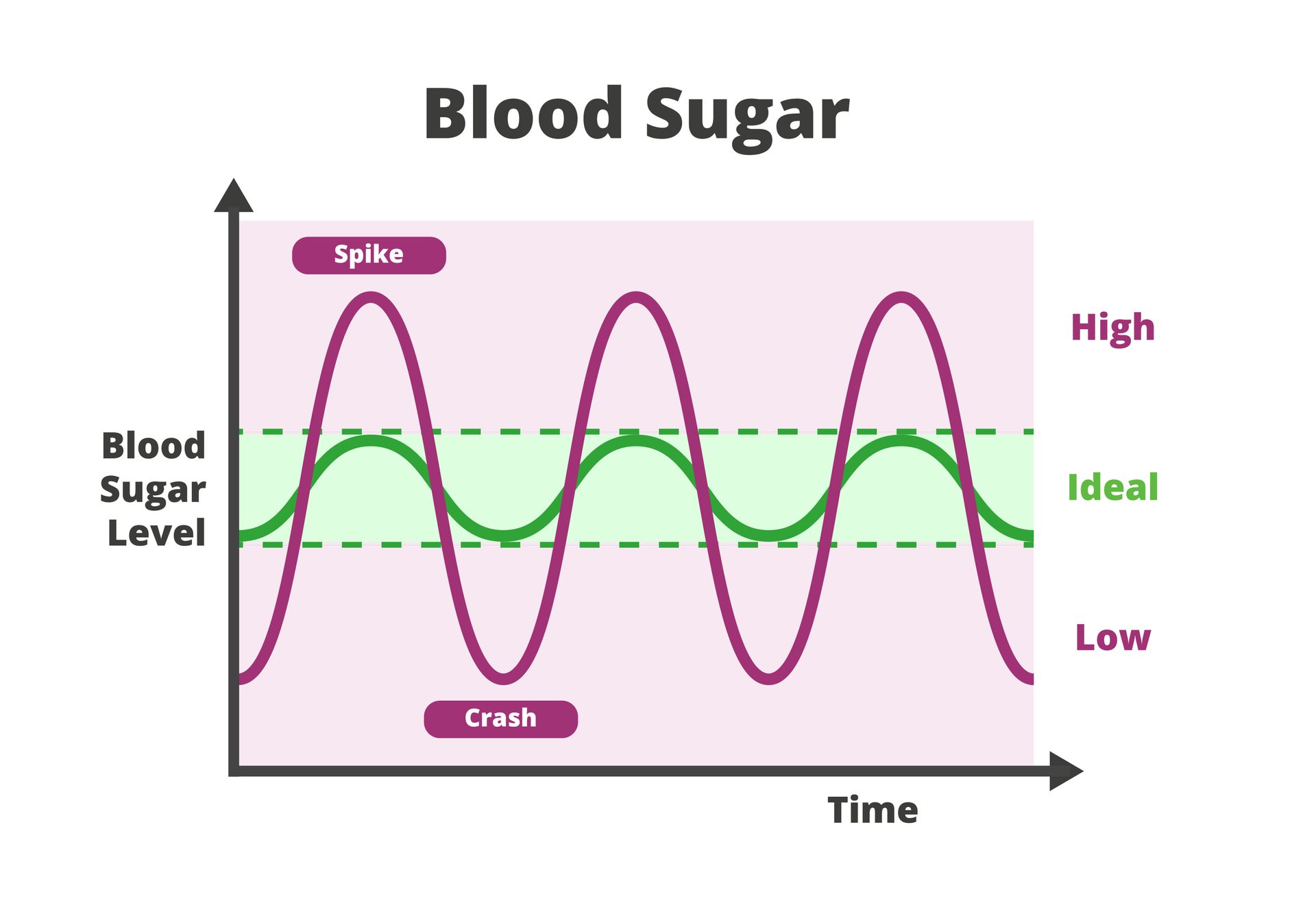
GLP‑1 (glucagon-like peptide‑1) agonists mimic a natural hormone produced in the gut. They help:
- Stimulate insulin production after meals (lowering blood sugar)
- Slow gastric emptying (so patients feel full longer)
- Reduce appetite through direct effects on the brain
While originally approved for type 2 diabetes, some GLP‑1s, such as Saxenda, Wegovy and Zepbound, carry FDA approval for weight loss in adults with a BMI of 30 or more, or 27 with other health issues like high blood pressure or cholesterol.
When Are They Prescribed?
For type 2 diabetes, GLP‑1s such as Ozempic, Rybelsus, Victoza, Trulicity and Mounjaro are commonly prescribed when lifestyle changes or metformin aren’t enough. They also offer cardiovascular benefits and lower the risk of hypoglycemia.
For weight management, medications like Wegovy and Zepbound are FDA‑approved for obesity treatment when:
- BMI is 30 or higher
- BMI is 27 or higher with weight‑related health conditions
- The patient has tried and failed non‑drug interventions such as diet and exercise
Cost and Why It’s Out of Reach for Many
At retail price, GLP‑1 medications can cost over $1,000 per month. That makes them difficult to afford for patients who rely on Medicaid or safety-net providers, unless insurance provides coverage. Even for patients who qualify for GLP-1s for weight loss, getting it covered can require extra steps, like providing documentation of previous failed weight loss attempts.
While the popularity of these drugs continues to grow, their accessibility remains limited without a qualifying diagnosis.
How Medicaid Covers GLP‑1s in Texas
Texas Medicaid does cover GLP‑1 medications for treating type 2 diabetes, including drugs like Ozempic and Trulicity. However, coverage for weight-loss-specific brands like Wegovy, Zepbound or Saxenda is not guaranteed and is often not included.
Current Texas Medicaid guidelines generally require:
- A confirmed diagnosis of type 2 diabetes
- Prior authorization
- BMI documentation
- Evidence that other treatments have been attempted
In most cases, weight-loss-only indications are not covered under Texas Medicaid. That means patients must either have type 2 diabetes or fit into a rare exception category to receive these medications through Medicaid.
Private Insurance Coverage
Coverage for GLP‑1s through private insurance varies widely. Many plans do cover them for diabetes, but using them for weight loss usually requires:
- Proof of a BMI of 30 or more, or 27 with related conditions
- Documentation of past attempts to lose weight through diet and exercise
- Trial of other, less expensive weight-loss medications first
Even when covered, co-pays can still be high, and approval may require multiple steps and appeals.
Policy Landscape and Future Outlook
Across the U.S., Medicaid prescriptions and spending on GLP‑1s have risen sharply in recent years. However, Texas has not adopted broader coverage for weight-loss use. Although the federal government has proposed expanding Medicare and Medicaid coverage for obesity drugs, those efforts are still in early stages and face political hurdles.
For now, access to GLP‑1s for weight management remains limited to those with qualifying diagnoses, private insurance with strong benefits, or the financial means to pay out of pocket.
What Houston Patients Interested in GLP-1 Should Do
If you’re in Houston and wondering whether you may qualify for GLP‑1 medications, here are some practical next steps:
- Know your diagnosis and discuss options with your PCP. Diabetes-related use is much more likely to be covered.
- Keep documentation and note any previous attempts at weight loss or lifestyle changes.
- Check your insurance policy or speak with a provider to clarify your plan’s coverage.
- Ask about alternative medications; options like phentermine or Contrave may be easier to access.
- If you have private (non-government) insurance, you may be eligible for drug manufacturer discount or copay savings programs.
- Stay informed about policy changes that may expand coverage in the future.
Explore Healthy Weight Management Options and Diabetes Treatments in Houston
For some patients seeking a GLP-1 prescription, even those who meet the BMI requirements, the process may still lead to a denial due to strict insurance rules or limited coverage. However, even if a GLP-1 drug isn't currently an option, our primary care doctors can work with you to build a manageable and effective weight management plan that fits your goals and budget.
Give us a call at (713) 778-1300 or contact us at St. Hope Healthcare today here on our website to schedule an appointment and learn about your options.