Recent Posts
When Blood Sugar Abnormalities Point to Something Other Than Diabetes
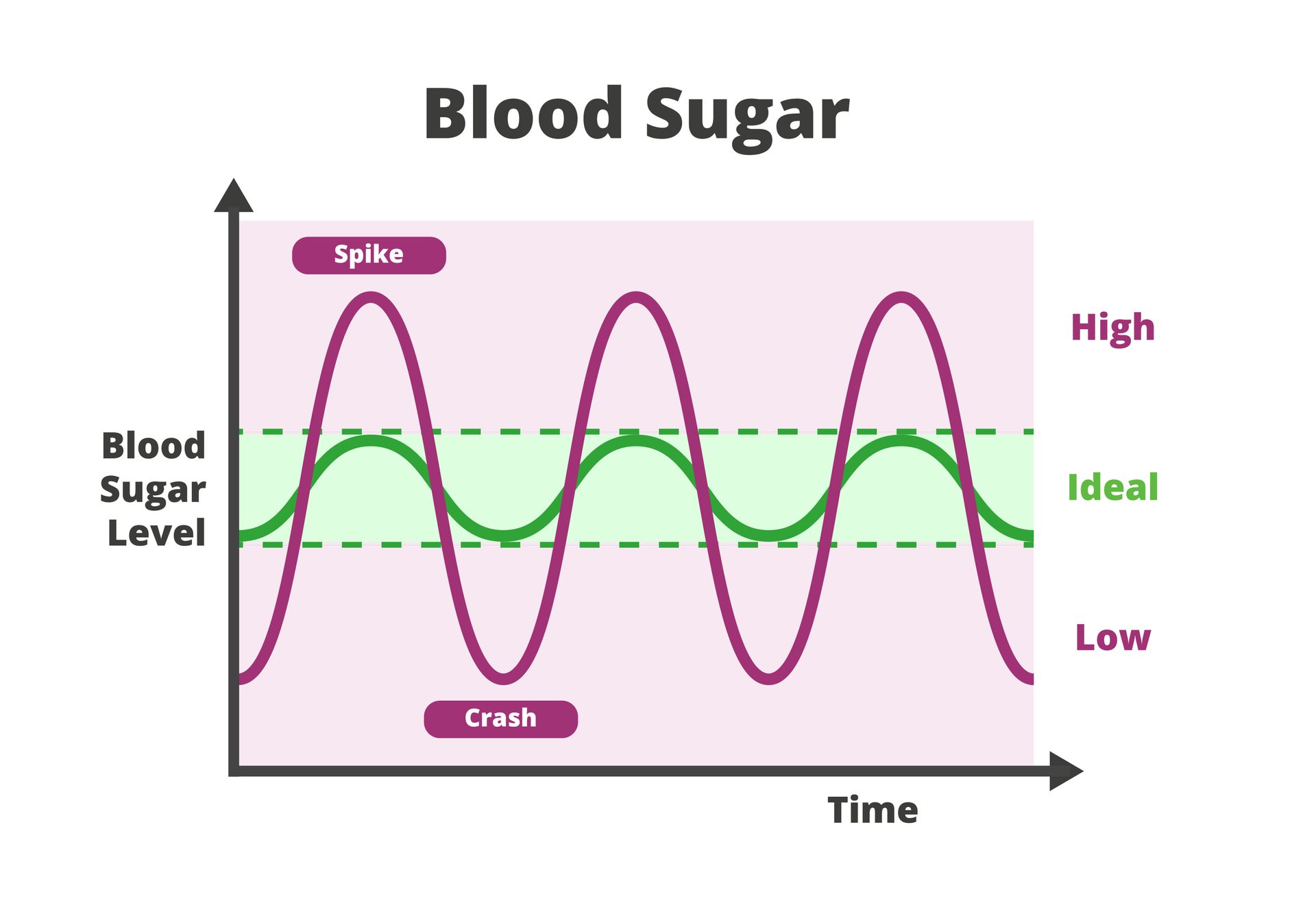
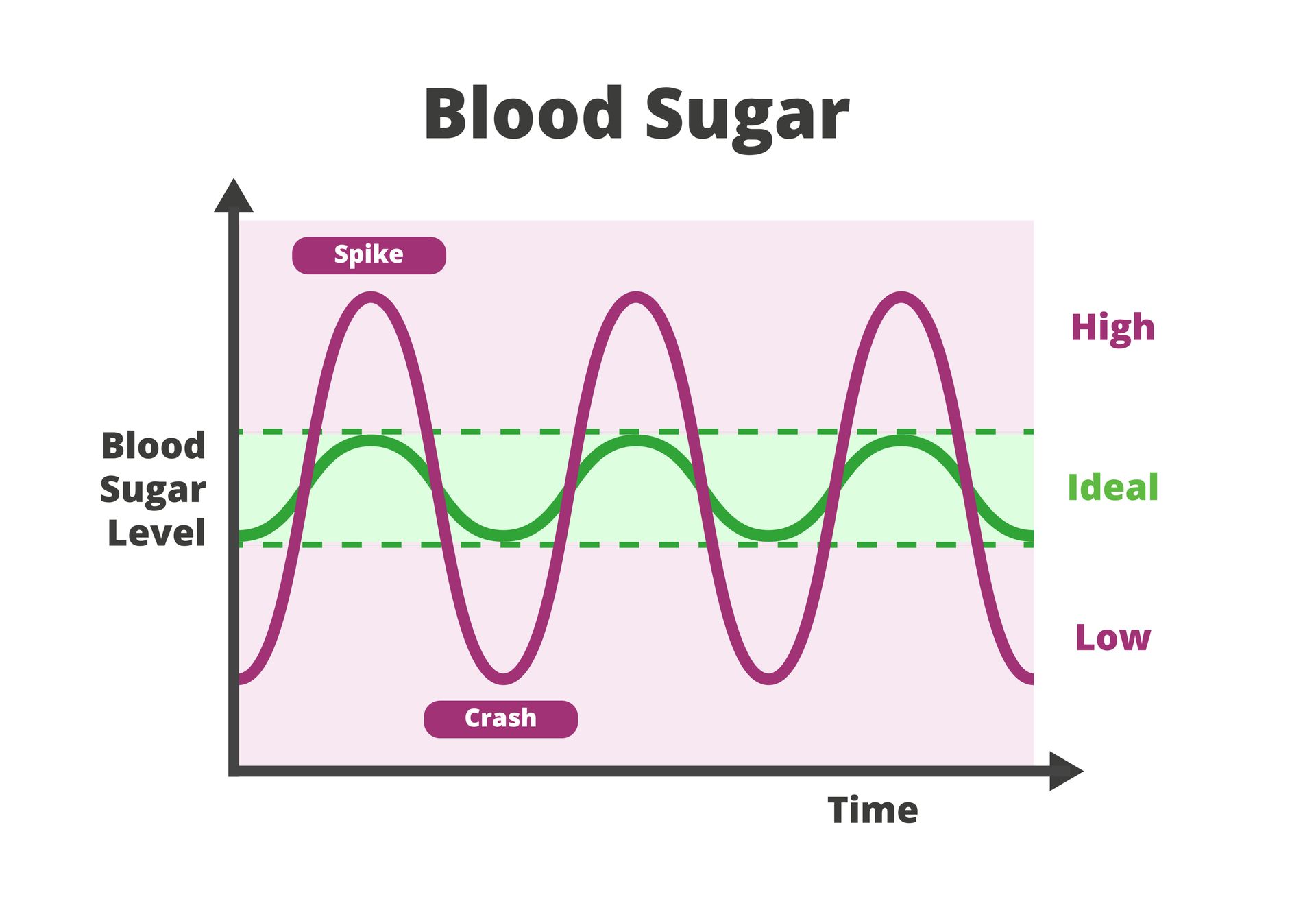
Many people immediately worry about diabetes when they receive abnormal blood sugar test results, but there can be other causes of elevated or irregular glucose levels. In primary care, clinicians often see temporary or situational blood sugar changes caused by stress, illness, medications or other short-term physiologic responses.
Stress Can Temporarily Raise Blood Sugar
The body’s stress response is powerful and fast. When you’re under physical or emotional stress, your adrenal glands release hormones like cortisol and epinephrine (adrenaline). These hormones are designed to mobilize energy, which includes raising blood glucose so cells have quick fuel.
Common stressors that can spike blood sugar include:
- Acute anxiety or panic episodes
- Poor sleep or sleep deprivation
- Intense physical pain
- Anxiety about the test itself, especially when diabetes is a concern
- Emotional stress from work, relationships or major life events
In these cases, blood sugar may be elevated on a single lab draw or fingerstick but return to normal once the stressor resolves. This is especially common when labs are drawn during urgent visits or after a rough night of sleep.
Primary care providers often recommend repeating testing under calmer, fasting conditions before drawing conclusions.
Illness and Inflammation Can Skew Results
Infections and inflammatory conditions frequently cause short-term blood sugar changes, even in people with no history of glucose issues.
When the body is fighting illness, it releases inflammatory cytokines and stress hormones that:
- Reduce insulin sensitivity
- Increase glucose production by the liver
- Slow glucose uptake into cells
This is why elevated blood sugar is common during:
- Viral or bacterial infections
- Fevers
- Post-surgical recovery
- Severe allergic reactions
Once the illness resolves, glucose levels often normalize on their own. Clinicians look closely at timing, when the test was drawn relative to symptoms, to determine whether follow-up testing is needed.
Medications Are a Frequent and Overlooked Cause
Certain medications can raise blood sugar temporarily or persistently without indicating diabetes. Common examples include:
- Steroids (prednisone, dexamethasone, inhaled corticosteroids at high doses)
- Decongestants containing pseudoephedrine
- Some antidepressants and antipsychotics
- Hormonal therapies, including certain birth control methods
- IV fluids containing dextrose
Steroid-induced hyperglycemia is particularly common and often reversible once the medication is stopped or tapered.
Providers will typically ask about recent prescriptions, injections or over-the-counter medications before interpreting results.
Non-Fasting Tests Can Be Misleading
Not all blood sugar tests are created equal. A random glucose reading, especially after eating, doesn’t carry the same diagnostic weight as a properly timed test. Blood sugar may appear elevated if:
- The test wasn’t fasting
- You ate a high-carbohydrate meal beforehand
- The blood draw occurred shortly after exercise or caffeine intake
This is why clinicians often rely on a pattern of results, not a single number. Follow-up testing may include:
- Fasting blood glucose
- Hemoglobin A1C (which reflects average levels over the past 3 months)
- Repeat labs under standardized conditions
One abnormal value alone rarely leads to a diagnosis.
Hormonal and Metabolic Shifts Can Play a Role
Blood sugar is influenced by multiple hormone systems, not just insulin. Temporary elevations can occur during:
- Pregnancy or postpartum hormonal shifts
- Thyroid dysfunction
- Menopause or perimenopause
- Polycystic ovary syndrome (PCOS)
In these cases, glucose abnormalities may be part of a broader metabolic picture rather than diabetes itself. Primary care providers look at symptoms, family history and related labs to determine next steps.
Dehydration and Lab Variability Matter
Even mild dehydration can concentrate glucose in the bloodstream, making levels appear higher than they truly are. This is especially common when labs are drawn:
- During illness
- After vomiting or diarrhea
- Following prolonged fasting
- In hot weather or after intense exercise
Lab variability also exists, and no test is perfect. That’s why repeat testing is often recommended before labeling a result as abnormal.
Why Context Matters More Than a Single Number
Primary care clinicians are trained to interpret blood sugar in context:
- Was the patient sick or stressed?
- Were medications involved?
- Was the test fasting?
- Are there symptoms suggesting diabetes?
Jumping straight to conclusions can lead to unnecessary anxiety and overtreatment. Thoughtful evaluation helps distinguish between temporary fluctuations and true metabolic disease.
Thoughtful Blood Sugar Evaluation Starts With Consistent Primary Care
At St. Hope Healthcare, our providers take a comprehensive, patient-centered approach to abnormal lab results. Rather than reacting to a single number, our Houston primary care team looks at stress levels, recent illness, medications and overall health to determine what’s actually happening and what, if anything, needs to be done next.
If you’ve received an unexpected blood sugar result or have concerns about metabolic health, contact St. Hope Healthcare at (713) 778-1300 to schedule a consultation or give us a call.