Recent Posts
Why Primary Care Providers Still Care About Symptoms That Resolved on Their Own

It’s a common moment in primary care visits: a patient mentions a symptom but adds, “It already went away, so I don’t know if it matters.” From the patient’s perspective, resolved symptoms can feel irrelevant. If it’s gone, why bring it up?
From a primary care provider’s perspective, those resolved symptoms can be very important. Primary care isn’t just about treating what’s happening today; it’s about understanding patterns over time and identifying early signals that put current health into context. Even symptoms that disappear on their own can offer valuable clues.
Resolved Symptoms Help Reveal Patterns, Not Isolated Events
Primary care focuses less on single moments and more on trajectories. A symptom that occurs once and never returns may not raise concern, but when similar symptoms appear repeatedly over months or years, they can point to an underlying process. For example:
- Occasional dizziness may seem harmless, but repeated episodes over time could suggest blood pressure variability, dehydration patterns or medication effects.
- Short-lived abdominal pain may not be alarming once, but recurring episodes could signal gallbladder issues, food intolerance or inflammatory conditions.
When providers document resolved symptoms, they can later identify whether changes in health are truly new or part of a longer pattern that’s only now becoming clearer.
Timing, Duration and Recurrence Still Matter
Even when a symptom resolves, how and when it happened remains clinically meaningful. Providers often want to know:
- When did it start?
- How long did it last?
- Did it resolve suddenly or gradually?
- Has it happened before?
A headache that lasted two hours once is very different from one that recurred daily for two weeks and then stopped.
Chest discomfort that resolved after rest may be evaluated differently than pain that resolved without explanation.
Primary care providers use this timeline information to assess risk, rule out serious conditions and decide whether monitoring or further evaluation is warranted, even if no action is needed immediately.
Some Symptoms Can Resolve, But Still Signal an Underlying Issue
Not all health issues cause continuous symptoms. Some conditions are episodic, meaning symptoms come and go, sometimes disappearing completely between episodes. Examples include:
- Heart rhythm disturbances that self-correct
- Mild asthma or airway reactivity
- Gallbladder or kidney stone irritation before obstruction
- Autoimmune or inflammatory conditions with flare-and-remission patterns
- Hormonal shifts that cause temporary symptoms
In these cases, symptom resolution doesn’t mean the issue is gone; it means it’s currently inactive. Documenting earlier episodes helps providers recognize these patterns if symptoms return or evolve.
Resolved Symptoms Provide Context for Future Complaints
One of the most valuable roles of primary care is continuity. When new symptoms arise, providers rely heavily on past history to interpret what’s happening now. For example:
- New fatigue may be interpreted differently if a patient previously reported unexplained weight changes or sleep disturbances.
- New pain may be contextualized by earlier episodes in the same location.
- New lab abnormalities may make more sense when paired with previously reported symptoms that resolved without treatment.
Without documentation of past symptoms, providers are forced to evaluate new complaints in isolation. When a provider knows the patient and their history, they can connect the dots more accurately.
Self-Resolving Symptoms Don’t Always Mean “Nothing Happened”
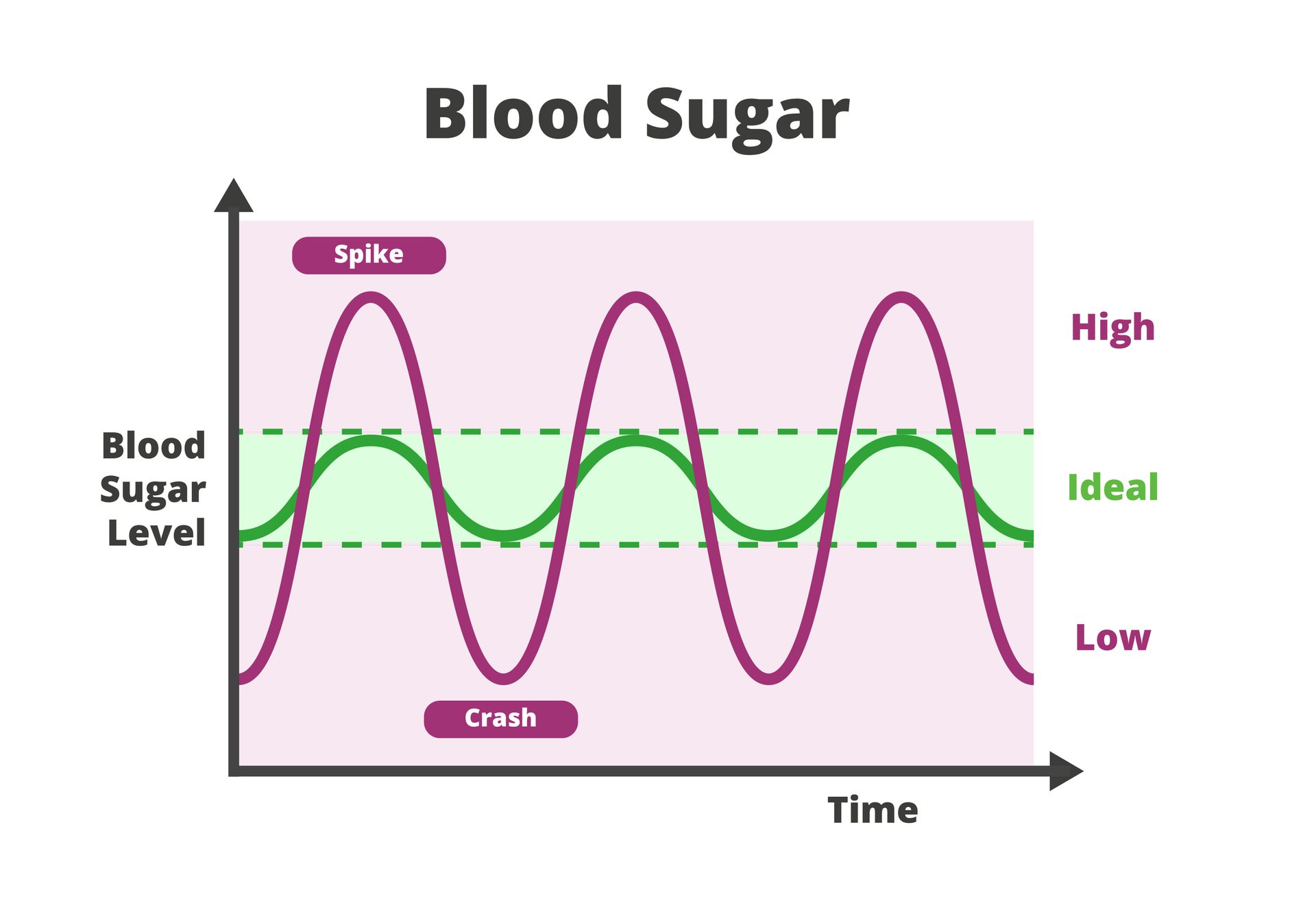
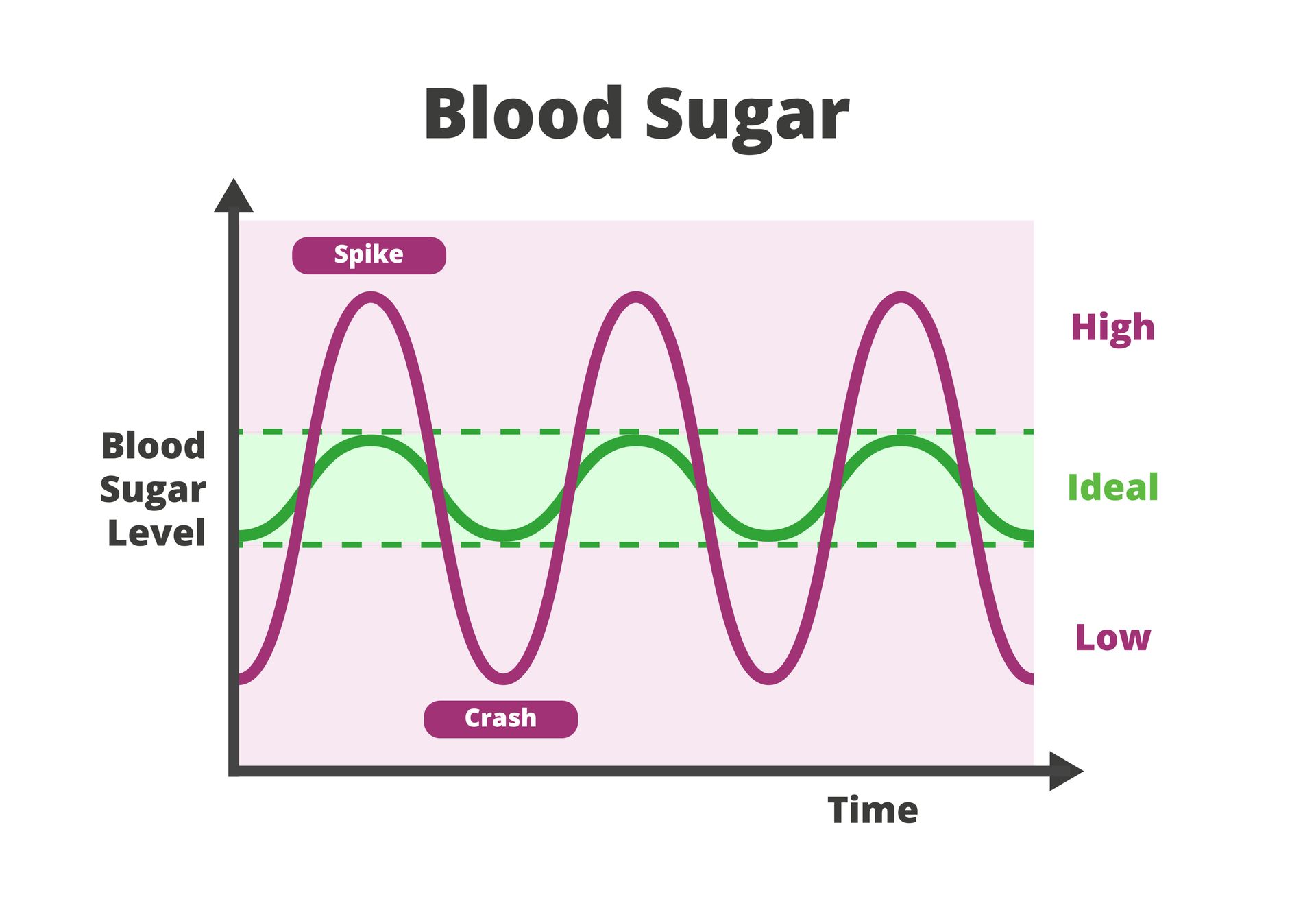
The body is very good at compensating. Many symptoms resolve because the body adapts, not because the cause disappeared. For instance:
- Blood pressure may normalize temporarily despite underlying cardiovascular stress
- Blood sugar may return to normal after short-term elevation
- Inflammation may quiet down before flaring again
Primary care providers understand that resolution doesn’t always equal resolution of risk. That’s why they listen carefully even when symptoms have passed.
Documentation Helps Avoid Over-Testing and Under-Testing
It might seem counterintuitive, but documenting resolved symptoms can actually reduce unnecessary testing. Providers may feel more confident monitoring rather than immediately ordering imaging or labs if they know a symptom has:
- Happened before
- Resolved without progression
- Remained stable over time
At the same time, documentation helps prevent under-testing when patterns suggest something more serious.
What Patients Can Do
You don’t need to overanalyze every ache or twinge, but it is helpful to mention:
- Symptoms that felt unusual, even if brief
- Symptoms that recur intermittently
- Symptoms that resolved but were intense or disruptive
- Anything that felt different from your usual baseline
Your provider can decide what’s relevant. Sharing the information allows them to do their job more effectively.
Primary Care in Houston That Looks at the Whole Picture
At St. Hope Healthcare, our primary care providers take a comprehensive, long-term view of health. If you have questions about past symptoms, ongoing concerns or how your health history fits together, contact St. Hope Healthcare at (713) 778-1300 to schedule a consultation or give us a call.