Recent Posts
Why Primary Care Providers Recommend More Frequent Blood Sugar Checks With Certain Medications

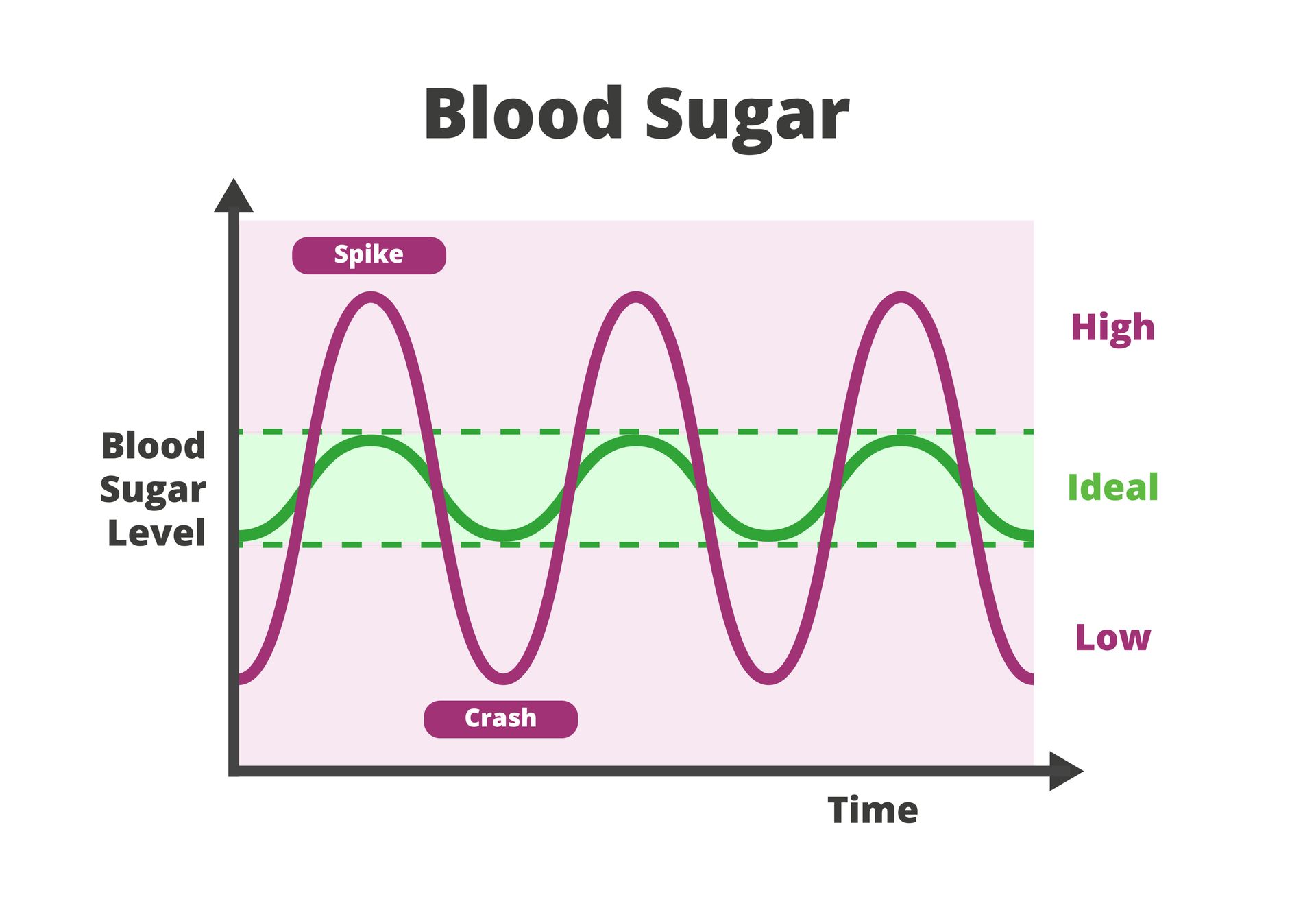
For people managing diabetes or prediabetes, blood sugar testing is a routine part of care.
Some medications affect glucose levels or how the body responds to insulin, which may make more frequent monitoring appropriate.
Your doctor’s recommendation to increase monitoring is not necessarily a sign that something is wrong. In many cases, it is a proactive step to understand how a medication interacts with your body and whether additional steps need to be taken to keep your blood sugar levels within a safe range.
How Medications Influence Blood Sugar Levels
Blood sugar regulation depends on a balance between insulin, hormones, liver function, diet and activity. Certain medications can disrupt that balance in subtle or temporary ways. Some medications may:
- Increase insulin resistance
- Change how much glucose the liver releases
- Affect appetite or digestion
- Influence how the body responds to insulin
- Mask symptoms of low blood sugar
Because these effects vary between individuals, monitoring provides valuable insight into how a specific medication affects each patient.
Steroids and Their Impact on Glucose
Corticosteroids are one of the most common medication groups associated with increased blood sugar levels. These medications are often prescribed to reduce inflammation, treat autoimmune conditions, manage asthma or address allergic reactions.
Steroids can cause the liver to release more glucose into the bloodstream while reducing the body’s sensitivity to insulin. As a result, blood sugar levels may rise, even in people who normally have good glucose control.
Healthcare providers often recommend more frequent monitoring during steroid treatment to track changes early and adjust care plans if needed.
Mental Health Medications and Metabolic Changes
Some medications used to support mental health can affect metabolism over time. These changes may influence weight, appetite or insulin sensitivity, which can indirectly affect blood sugar levels.
The effects may develop gradually rather than immediately. Increased monitoring helps healthcare providers identify trends before they become more difficult to manage. This approach supports long-term health without interrupting mental health treatment unnecessarily.
Blood Pressure and Heart Medications
Certain heart and blood pressure medications can affect how the body responds to low blood sugar episodes. While they may not directly raise glucose levels, they can reduce common warning signs such as shakiness or rapid heartbeat.
When these symptoms are less noticeable, low blood sugar episodes may go unrecognized. More frequent monitoring helps ensure that glucose levels remain stable even when physical cues are subtle.
Medications That Affect Appetite or Digestion
Some prescriptions alter appetite, slow digestion or change how nutrients are absorbed.
When eating patterns shift, blood sugar levels often shift as well.
Monitoring during these changes helps determine whether glucose levels remain balanced throughout the day. It also supports better meal planning and medication timing, especially during the adjustment period after a patient begins taking a new medication.
Dose Changes and Medication Transitions
Even medications a patient has taken before can affect blood sugar differently when doses are increased or decreased. Starting, stopping or adjusting medications may temporarily alter glucose patterns.
Healthcare providers often recommend short-term increases in monitoring during these transitions. This allows for timely adjustments and reduces the risk of prolonged high or low blood sugar levels.
Why Monitoring Is a Preventive Measure
Medication effects on blood sugar are highly individual. Two patients taking the same medication may experience very different results based on age, activity level, diet and overall health. More frequent blood sugar monitoring allows your primary care provider to:
- Identify patterns before symptoms develop
- Prevent extended periods of imbalance
- Fine-tune medication plans
- Support safer long-term treatment decisions
Rather than reacting to symptoms after they occur, monitoring helps guide care proactively.
Communicating Results With Your Provider
Blood sugar monitoring is most effective when results are shared. Keeping a simple record of readings, along with notes about medication timing and meals, helps your healthcare team understand the full picture.
In most cases, increased monitoring is temporary and focused on learning how a medication affects the body. Once patterns are clear, you may be able to return to your previous monitoring schedule.
Get Advice on Blood Sugar Monitoring From Our Houston Doctors and Family Nurse Practitioners
St. Hope Healthcare provides patient-centered care and personalized guidance for managing diabetes, including advice on monitoring blood sugar after starting new medications. Call us at (713) 778-1300 to schedule an appointment at one of our health centers in Houston, Bellaire, Conroe, Sugar Land and Dickinson.